What does it mean for the people?
Epidemiological data science, including collation of data and analysis and publishing such analysis in simple infographics, is key to making people understand the nature and extent of the impact of COVID-19 on the lives of people. It helps governments and policy makers in contingency planning, drafting of guidelines and protocols, and enforcing those guidelines. It helps ordinary people comprehend the whole situation and prepares them for any eventuality. Making all facts and options known to everyone gives them the power to decide on the course of action they will take, how to do it, and whether or not they will act upon the options they have chosen.
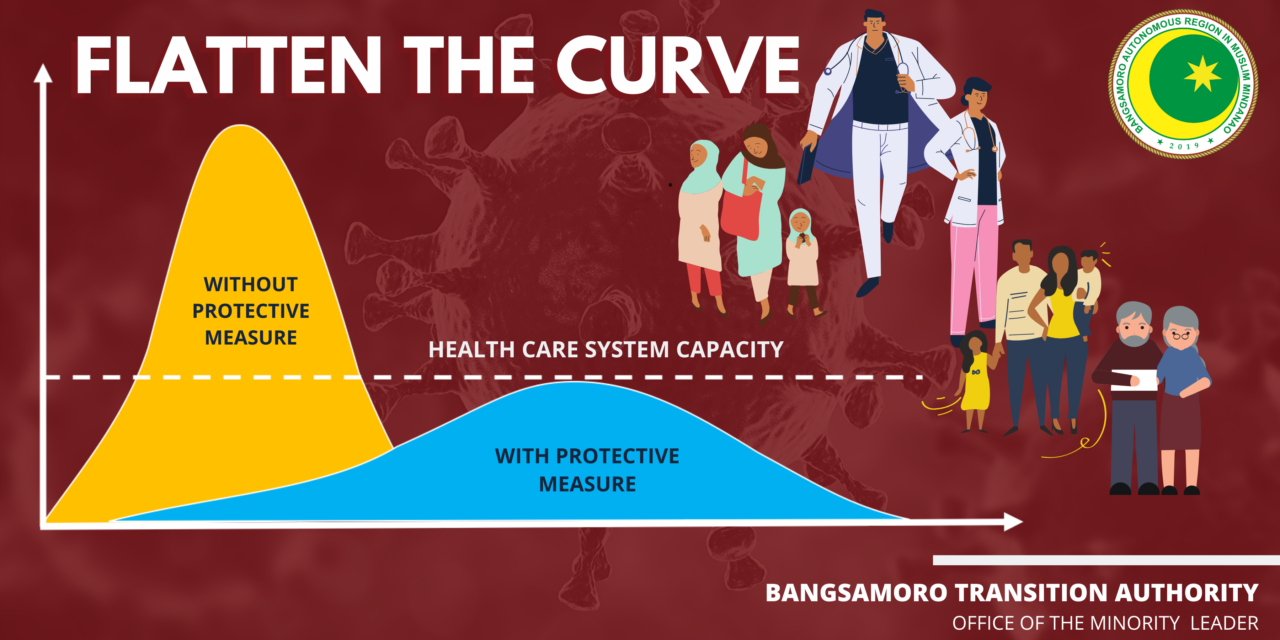
What do we mean when we say “flatten the curve?”
This is how COVID-19 looks like on a graph. COVID-19 cases start small in a community or country. When there are no protective measures to SLOW DOWN the rate of infection, the number of people infected with the virus goes up exponentially. When this happens, hospitals and the entire health care system in the community or country are overwhelmed and burdened beyond their capacity. When there are more patients coming in compared to the number of beds, ventilators, equipment and medical front-liners, the healthcare system breaks down. People will die in record numbers, just like what happened in Italy. Doctors, nurses, respiratory therapists and other health workers themselves will be infected and would need to go into isolation or quarantine. Even countries with more advanced healthcare systems compared to the Philippines, such as Italy, have been overwhelmed by the sheer number of COVID-19 patients. Sadly, we see this in Metro Manila now. Our doctors are dying, medical personnel are becoming PUIs and PUMs and need to undergo quarantine. What will happen when there will be no more medical front-liners to treat and help the patients?
In other parts of the country such as in BARMM, there’s less capacity — Less number of hospital beds; minimal number of ICU beds, ventilators (which are needed for moderate to severe cases of COVID-19), disinfection chambers, and personal protective equipment (PPEs) for medical front-liners; minimal to zero number of testing kits in hospitals and RHUs; and no testing laboratories. There is also, to date, no government-prescribed algorithm for treatment of COVID-19 patients yet. While there’s research and literature on possible institutional treatment and management options for COVID-19 based on other countries’ experiences, our heroic doctors and the entire medical community would need to be innovative and implement as promptly as possible any and all clinical management measures that are appropriate and available for the patient, considering the rapid progression of the disease.
Considering this scenario, there is an imperative need to delay the spread of the contagion so as not to overwhelm the healthcare system of the country. How do we lower the number of patients and delay the corona virus peak (see graph)?
FLATTEN THE CURVE to reduce the burden on hospitals to the level where they are able to sufficiently and timely respond to, treat, and appropriately manage COVID-19 patients.
This is the most imperative reason why LGUs are enforcing lockdowns, enhanced community quarantines, general quarantines, and why national government declared a national public health emergency. Other protective measures include social distancing, staying at home, prohibition on mass gatherings, regulating travels, closure of non-essential establishments where people are likely to converge. There’s also a need to strengthen the capacity of hospitals all over the country to manage COVID-19 patients, thus, the use of calamity funds to purchase much needed PPEs, medicines, ventilators, and other medical facilities and equipment. LGUs must also identify institutional quarantine areas for the expected surge in PUIs and PUMs when it is deemed no longer safe to let them do self-quarantines at home in order to totally stop the spread of the virus. Hotels, hostels, gyms and other buildings with beds and rooms can be taken over by LGUs (with appropriate cost) and utilised as separate quarantine areas for PUIs and as extensions of hospitals treating positive cases once the number of cases will rise.
In the meantime, while people are on strict home quarantines, both government and the private sector must work on helping the daily wage earners and those below the poverty line by providing social amelioration packages including food packs and medicine, release of salaries and portions of bonuses, delaying payment of rents, among others. Transportation must be provided to frontline medical workers, including other workers who need to continue working such as those in banks, grocery stores, pharmacies, government offices, policemen and firemen, janitors and other utility workers.
All these protective and preventive measures are already being enforced now. And the least we all can do is to abide by the guidelines enforcing these measures.
Everyone, please cooperate and help slow down the contagion. Help flatten the curve. Be a hero and save the lives of other people. Strengthen your immune systems. Stay indoors. STAY HOME.